The Role of Stem Cell Culture Media in Regenerative Medicine
August 12, 2025Introduction
Stem cells are the body’s raw building blocks — undifferentiated cells with the remarkable ability to develop into specialized cell types. Unlike most cells in the body, which have specific roles and a limited ability to divide, stem cells can both self-renew (make identical copies of themselves) and differentiate (transform into other cell types).
These unique properties make stem cells central to life itself: they drive early development, maintain healthy tissues, and hold immense promise for treating diseases that were once considered incurable.
Over the past few decades, advances in stem cell research have reshaped medicine. Scientists have discovered ways to grow stem cells in laboratories, reprogram adult cells into stem-like states, and use them to repair damaged tissues. As a result, stem cells are no longer just a subject of academic curiosity, they’re becoming a practical tool in regenerative medicine, drug discovery, and disease modeling.
What Makes Stem Cells Unique?
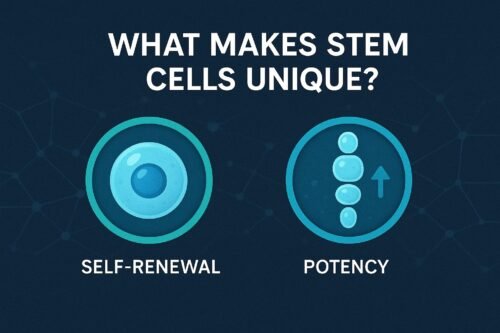
Stem cells are defined by two fundamental characteristics:
Self-Renewal
Stem cells can divide and produce copies of themselves over long periods, sometimes for the lifetime of an organism.
Example: Hematopoietic stem cells in bone marrow continuously generate new blood cells throughout life.Potency
Potency describes a stem cell’s ability to differentiate into other cell types:Totipotent: Can produce all cell types, including extraembryonic tissues like the placenta.
Pluripotent: Can produce almost any cell type in the body but not the placenta.
Multipotent: Can produce several cell types within a specific lineage.
Unipotent: Can produce only one type of cell but still has self-renewal ability.
Historical Background
The concept of stem cells dates back more than a century. In the late 19th century, scientists proposed the existence of cells with regenerative potential. By the 1960s, Canadian scientists Ernest McCulloch and James Till provided the first concrete proof of stem cells by identifying hematopoietic stem cells in mouse bone marrow.
The next big leap came in 1998, when human embryonic stem cells (ESCs) were first isolated, opening new possibilities for regenerative medicine — and sparking ethical debates that continue today. In 2006, Shinya Yamanaka’s discovery of induced pluripotent stem cells (iPSCs) revolutionized the field by showing that adult cells could be “reprogrammed” to an embryonic-like state without using embryos.
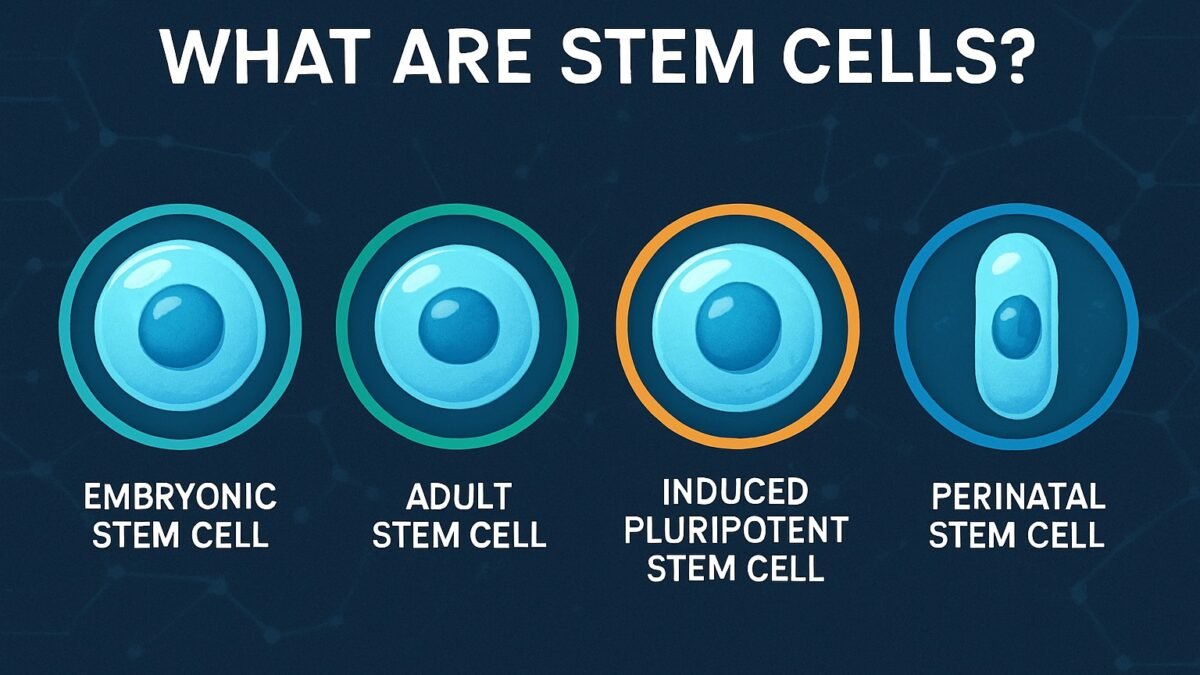
Main Types of Stem Cells
1. Embryonic Stem Cells (ESCs)
Source: Extracted from the inner cell mass of a blastocyst (an early-stage embryo about 4–5 days after fertilization).
Potency: Pluripotent — can form over 200 different cell types.
Advantages: Highest versatility for regenerative medicine; stable growth in culture.
Applications:
Modeling human development in the lab.
Testing drug safety and toxicity.
Potential treatments for degenerative diseases (e.g., Parkinson’s, macular degeneration).
Limitations:
Ethical concerns about embryo destruction.
Risk of immune rejection if cells come from a donor.
Potential to form tumors (teratomas) if not fully differentiated before use.
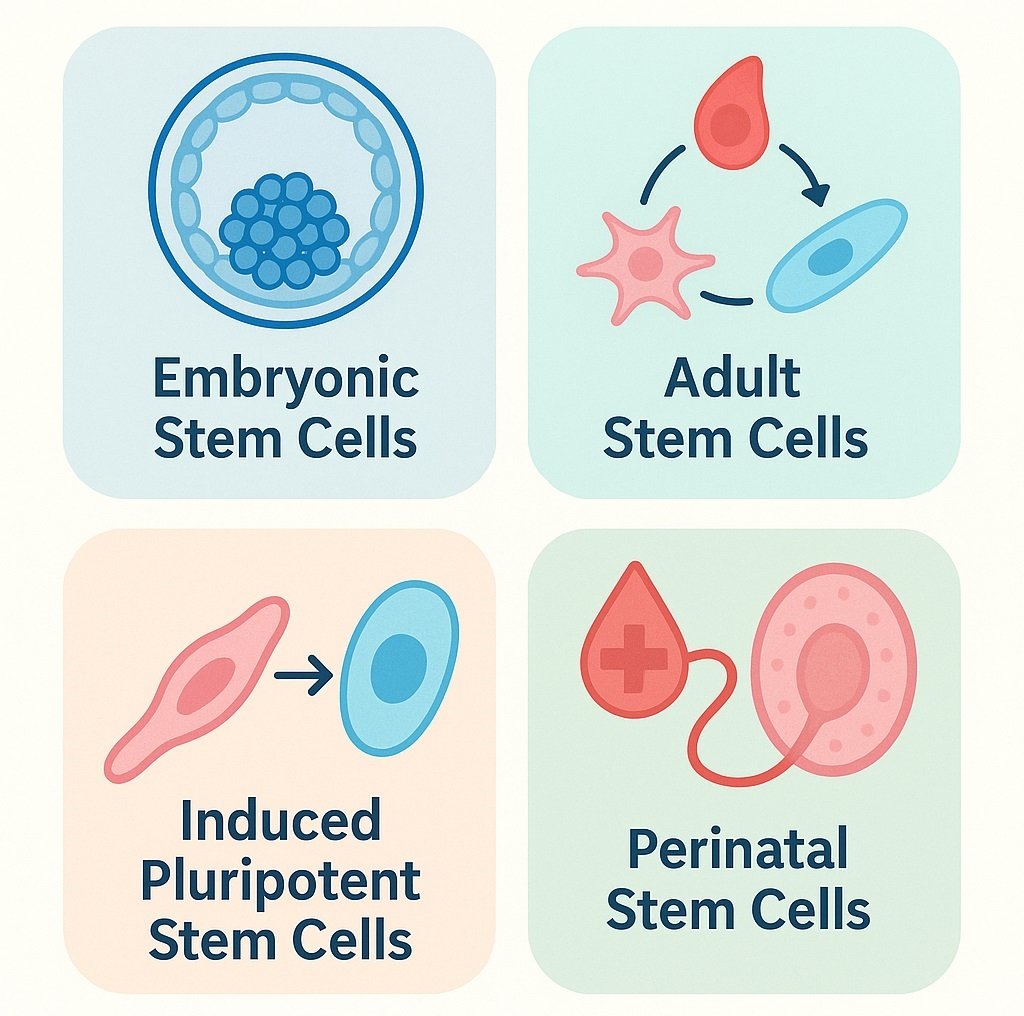
2. Adult (Somatic) Stem Cells
Source: Found in various tissues, where they maintain and repair the tissue.
Potency: Mostly multipotent.
Subtypes:
Hematopoietic Stem Cells (HSCs): Produce red blood cells, white blood cells, and platelets. Used in bone marrow transplants for leukemia and lymphoma treatment.
Mesenchymal Stem Cells (MSCs): Can become bone, cartilage, muscle, fat, and connective tissue. Found in bone marrow, fat, and umbilical cord tissue.
Neural Stem Cells: Found in specific brain regions; can generate neurons, astrocytes, and oligodendrocytes.
Epithelial and Epidermal Stem Cells: Regenerate skin and lining tissues.
Advantages: Lower ethical concerns; reduced risk of immune rejection if from the same patient.
Limitations: Restricted potency compared to embryonic stem cells; harder to expand in large numbers.
3. Induced Pluripotent Stem Cells (iPSCs)
Source: Adult cells (e.g., skin fibroblasts) genetically reprogrammed to a pluripotent state.
Potency: Pluripotent.
Advantages:
Avoids use of embryos.
Can be patient-specific, minimizing rejection risk.
Useful for modeling patient-specific diseases.
Applications:
Personalized medicine (e.g., creating heart cells from a patient’s skin cells for drug testing).
Studying genetic disorders in a dish.
Limitations: Potential for genetic instability and tumor formation if not carefully screened.
4. Perinatal Stem Cells
Source: Umbilical cord blood, placental tissue, and amniotic fluid collected at birth.
Potency: Multipotent (some show broader potential).
Advantages:
Easily collected without harm to mother or baby.
Cord blood stem cells can be banked for future medical use.
Applications:
Treating blood disorders like thalassemia and sickle cell anemia.
Immune system reconstitution after chemotherapy.
Potency Levels in Detail
| Potency | Definition | Examples | Applications |
|---|---|---|---|
| Totipotent | Can form all cell types, including placenta | Zygote, early embryonic cells | Complete organism development |
| Pluripotent | Can form all body cell types but not placenta | ESCs, iPSCs | Regenerative medicine, disease modeling |
| Multipotent | Can form several related cell types | HSCs, MSCs | Tissue repair, specific transplants |
| Unipotent | One cell type only | Muscle stem cells | Single-tissue regeneration |
Current and Emerging Applications
Regenerative Medicine: Repairing damaged tissues (heart muscle post-heart attack, neurons in Parkinson’s disease).
Drug Discovery & Toxicology: Screening new compounds on human-derived cells.
Disease Modeling: Reproducing diseases in lab-grown tissues to study their mechanisms.
Gene Editing with CRISPR: Correcting mutations in patient-derived stem cells before reintroducing them.
Organ Bioengineering: Using stem cells to grow tissues and organs in the lab.
Challenges and Ethical Considerations
Ethics of Embryonic Stem Cells: Debate over using embryos for research.
Tumor Risk: Pluripotent cells can form teratomas if not fully differentiated.
Immune Rejection: Cells from donors may be attacked by the recipient’s immune system.
Standardization: Ensuring consistent quality and safety across laboratories.
The Future of Stem Cell Research
The next decade is expected to bring:
Fully functional lab-grown organs for transplant.
Safe and effective stem cell therapies for currently untreatable conditions.
Integration of stem cells with 3D bioprinting and organ-on-chip technologies.
Wider availability of patient-specific iPSC therapies.
Conclusion
Stem cells represent one of the most exciting frontiers in modern science. Understanding the different types, embryonic, adult, induced pluripotent, and perinatal, is essential for appreciating their potential and limitations. As research progresses, stem cells may redefine how we treat diseases, repair injuries, and even replace entire organs.
References:
National Institutes of Health. Stem Cell Basics.
Yamanaka, S. (2007). Induction of Pluripotent Stem Cells from Adult Human Fibroblasts. Cell.
Nature Reviews Molecular Cell Biology. Stem Cell Classifications and Potency.
Mayo Clinic. Stem Cell Therapies: Research and Applications.